Régulation de la Natrémie, ADH, SiADH, Diurèse,
voir aussi le topo HypoNa non urgente
Le rein élimine normalement trés bien l'eau: une hypoNa donc résulte de:
Les étiologies les plus fréquentes:

Voir les autres causes plus bas.
aSymptomatique si sup. à 125 ou si installation lente.
Iono Sang avec uricémie et osmolarité
Iono Urinaire (Na, K, G, Urée)
Le Na/K Urinaire dépendent:
Si Hypovolémie, le NaU devrait etre bas. Si hypoK, le Ku devrait etre bas.
Analyse:
To excrete free water, urinary sodium plus urinary potassium must be less than the serum sodium concentration: NaU+KU < Na
NaU + Osmolarité urinaire:
Osmolarité urinaire = 2 (Na + K) + glucose + urée
Measuring urine osmolality is useful in ascertaining whether hyponatremic patients are making appropriately dilute urine (< 100 mOsm/kg). If they are, the cause of the hyponatremia may be excessive water intake, a reset osmostat, or low solute intake. In addition, patients with hypovolemic hyponatremia may have appropriately dilute urine soon after treatment with isotonic intravenous fluids.
The serum sodium concentration often returns to normal if the underlying cause is eliminated (eg, if excessive fluid intake is stopped).
Hormones Thyroïdiennes, en cas de clinique évocatrice
Cortisol sérique, en cas de clinique évocatrice
"fausse hypoNa": Une hyperG, perf de Glucosé hypertonique, perf de mannitol entrainent une hypertonie > 295 mOsm avec baisse de toutes les valeurs plasmatiques par brusque dilution du fait du transfert d'eau vers le secteur extra cellulaire, en particulier de la natrémie qui n'est alors plus le reflet de l'osmolalité plamatique. La valeur utilisable de la natrémie est:
Na+c = Na+m + (Gluc - 5.6) x 0.288 Where Na+c = Corrected plasma sodium (mmol/l) Na+m = Measured plasma sodium (mmol/l) Gluc = Measured plasma glucose (mmol/l)
Par contre, dans l'intox Alcoolique la diffusion fait que les osmoles apportées ne sont pas osmotiquement efficaces et n'entrainent donc pas d'hypoNa sauf intox massive et prolongée par la bierre.
Cf. HypoNaHyperOsm.pdf, Hyponatremia_evaluatingcorrectionfactorforHyperG.pdf,
Calcul de la tonicité (à différencier de l'osmolarité):
Tonicité = osmolarité efficace = 2Na + G égale à 285 mOsm/Kg dont 140 de Na et 5 de glucose (normale de 275 à 290).
Att: si on pense que l'urée est d'augmentation récente, il faut utiliser une formule qui en tient compte.
Résultat:
Most cases of hyponatremia that occur out of the hospital are chronic and minimally symptomatic, except in marathon runners, users of 3,4-methylenedioxymethamphetamine (MDMA, also known as "ecstasy"), and people who drink water to excess;
in these groups, severe symptoms usually indicate acute hyponatremia and require rapid correction.
"visual changes, focal neurologic changes, encephalopathy, respiratory depression, and seizures. Ultimately, brain herniation can occur."
Le cerveau sommence à s'adapter des les premieres minutes avec une adaptation complète en 2 à 3j.
2 stratégies
Hypertonic saline therapy should usually be discontinued well before the serum sodium level has risen this much, to avoid a continuing rise in the sodium level after the infusion has stopped.
Le schéma suivant reste à 1-2 ml/kg/h en cas de convulsion mais l'article est plus ancien (2007):
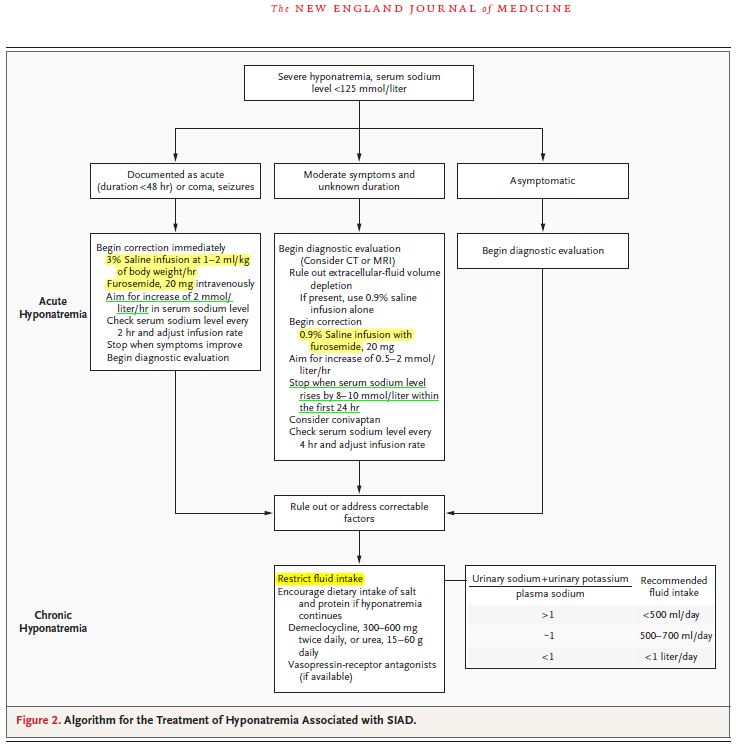
[NEJM 2007]
One approach is to aim for the cessation of neurologic symptoms, such as seizures, and then reduce the correction rate. An increase in serum sodium levels of less than 10 mmol per liter is usually sufficient to reduce the symptoms and prevent complications.
In patients with seizure and coma, it is reasonable to use 3% saline at a rate of 1 to 2 mmol per liter per hour, even if the hyponatremia has been present for longer than 24 hours, keeping the maximal correction to 8 to 12 mmol per liter per day.
[Cleveland]:
In patients having active seizures or showing signs of brain herniation, 3% saline can be given initially at a higher rate of about 2 to 3 mL/kg/hour over the first few hours.
An alternative approach is an initial 50-mL bolus of 3% saline and an additional 200 mL given over the subsequent 4 to 6 hours.
After severe signs and symptoms have resolved, 3% saline is promptly discontinued and appropriate therapy is initiated based on the patient’s volume status and underlying cause of hyponatremia.
Aggressive initial correction at the rate of 1.5 to 2 mmol/hour for the first 3 to 4 hours with 3% saline is indicated until serious symptoms (seizure, obtundation) resolve, but correction beyond 10 to 12 mmol/L in the first 24 hours should be avoided.
While hypertonic saline is being infused, serum sodium levels should be checked every 1 to 2 hours.
[NEJM 2007]
When milder symptoms are present, correction is generally slower (rate 0.5 mmol per liter per hour); some authorities avoid the use of 3% saline in this setting.
[Cleveland]
Patients with serious signs or symptoms should receive hypertonic (3%) saline at a
rate of about 1 mL/kg/hour for the first several hours.8 Those with concomitant hypervolemia (as in congestive heart failure) or underlying cardiovascular disease should also receive a loop diuretic to aid in free-water excretion and to prevent volume overload from the saline infusion. This regimen usually raises the serum sodium concentration enough (usually by about 1 mmol/L/hour) to decrease cerebral edema and improve symptoms.
Indication selon la présence de:
Vitesse de correction
Méthode de correction
Utiliser du NaCl 3% (hypertonique):
Autres protocoles:
La CAT est guidée par la volémie. Cf HypoNaNonUrgente
Thiazide diuretics should be discontinued and hypovolemia and hypokalemia should be corrected with isotonic saline and potassium supplementation. As the hypokalemia is corrected and the diuretic effect and hypovolemic stimulus to ADH dissipates, water excretion can increase rapidly, resulting in a brisk change in serum sodium. Serum sodium levels should be closely monitored during therapy to avoid overcorrection. For this reason, use of hypertonic saline should generally be avoided. Hypotonic fluid— eg, half-normal (0.45%) or quarter-normal (0.22%) saline or even desmopressin—may become necessary in the later stages of therapy to avoid overly rapid correction.
Consensus recommendations suggest that most patients with mild hyponatremia (serum sodium 130 to 135 mmol/L) should be treated with fluid restriction and clinical observation, as spontaneous water diuresis leads to improvement in the serum sodium level.
Importantly, the reflex to provide isotonic saline infusions should be avoided unless clear signs of volume depletion are present. Intravenous saline has the potential to worsen hyponatremia in the presence of ADH.
In addition, some athletes will have retained water in the gastrointestinal tract that may be mobilized after the race, resulting in worsening of hyponatremia. In athletes with severe hyponatremia (serum sodium < 120 mmol/L) or symptomatic exercise-associated hyponatremia (lethargy, respiratory depression, seizures), hypertonic saline is the treatment of choice. One protocol suggests giving 100 mL of 3% saline over 10 minutes in the field, followed by prompt transportation to hospital.
The focus of treatment remains water and salt restriction and judicious use of loop diuretics and aldosterone antagonists such as spironolactone (Aldactone).
As the severity of cirrhosis increases, the only effective treatment of hyponatremia is liver transplantation.
Cf. SiADH
In most cases, water restriction is the mainstay of therapy. Although fluid restriction is usually effective, many patients cannot adhere to the level of restriction required. In cases in which fluid restriction is not effective on its own, demeclocyline can be used to antagonize ADH action and increase water excretion. Sodium tablets and loop diuretics can also be used, taking care to avoid hypovolemia from diuretic-induced sodium losses.
La symptomatologie déficitaire apparait 3 jours aprés la correction trop rapide de l'hypoNa et une IRM est nécessaire pour la confirmer.[Osmolar Disorders]
When symptoms of osmotic demyelination develop
during the treatment of hyponatremia, case reports
suggest that it may be possible to reverse the neurologic deficits by again lowering the serum sodium
level. In two patients who had neurologic
symptoms after rapid correction of serum sodium
levels, symptoms diminished when serum sodium
levels were modestly reduced by administering
the vasopressin analogue desmopressin
(DDAVP, Rhone–Poulenc Rorer; Stimate, Centeon)
and 5% dextrose.
[Cleveland]
If the serum sodium concentration
has been overcorrected Desmopressin is effective in preventing and
reversing inadvertent overcorrection of hyponatremia.
In one study, desmopressin lowered
the sodium concentration by 2 to 9 mmol/L in 14 of 20 patients. None of the patients developed
any serious adverse consequences.
In addition, intravenous water (dextrose 5%) can be given alone or in combination with desmopressin to prevent or reverse an
excessive increase in serum sodium. Such
therapy may be considered in patients who
continue to excrete hypotonic urine and have
already reached a serum sodium concentration
that meets or exceeds the recommended
rate or magnitude of change.
entraine:
CAT
Du G5 chez un enfant: Le G5 pur est CI chez l'enfant. Il se comporte comme de l'eau pure. HypoNa, Convulsion, décés apres une perf d'1 litre.
Une femme de 32 ans, de 46 kg, fait 2 crises d’épilepsie en postopératoire: Elle avait reçu 3 litres de glucosé à 5 % en 24 heures et on ne sait combien elle a bu. Sa natrémie est de 112 mmoles/L, kaliémie 4,1 mM, glycémie 5 mM. La tonicité est donc de 229 mOsm/L et son Eau tot est de 23 litres (0,5 × 46). On veut monter sa natrémie de 3 mmoles en 3 heures (1 mmol/h pendant 3 h). On choisit du NaCl à 3 %. La formule d'Adrogué et Madias indique qu’un litre va faire monter la natrémie de 16,7 mmoles ([513] – [112]) / 23 + 1). Comme on ne veut que 3 mmoles, c’est 3/16,7 = 0,18 litre en 3 heures soit 60 ml par heure pendant 3 heures de NaCl à 3 % qui seront perfusés. Ensuite, une remontée plus lente devra être instituée (en fondant les modifications du type de perfusion et de sa vitesse toujours sur la même formule). Un contrôle biologique régulier est impératif.
Retirer 110 ml d'un litre de NaCl 0,9% et les remplacer par du NaCl 20% (Amp de 20ml donc 5,5 ampoules):
1. NaCl 0,9% soit 9 mg/ml
On en prend 890 ml, ce qui contient: 8010 mg
2. NaCl 20% soit 200 mg/ml
On en prend 110 ml, ce qui contient: 22000 mg
Au total on a donc 1000 ml contenant 30010 mg
soit 30,01 mg/ml ie NaCl à 3% cqfd...
"Exercise-Associated Hyponatremia"
HypoNa par: